Introduction
The world is evolving exponentially, and where everything is coming under the wave of this inevitable revolution, healthcare and medicine is no far behind. The advancement in telecom technologies has changed the way we communicate with each other and hence made this world a ‘global village’. As soon as the twentieth century began, we had stepped into an ever-so evolving Digital Age or New Media Age. Information and communication technology (ICT) has advanced itself more than ever in the past century (Darkins et al., 2000). This proliferation of technology has knocked on the doors of medical department as well. A lexicon of scientists and researchers are in continuous thinking process of how to utilize this evolving way of communication in context to improve and meliorate medicine and healthcare delivery. Telemedicine and telehealth are the products of this continuous accretion and amalgam of telecommunication and medical services which proceeds to grow day by day as more and more people become mindful as to how advantageous this piece of technology is. These technologies have not only affected our medical and social spectrum of beliefs but also have left a trace in our cultural and economic dimensions as well (Darkins et al., 2000).
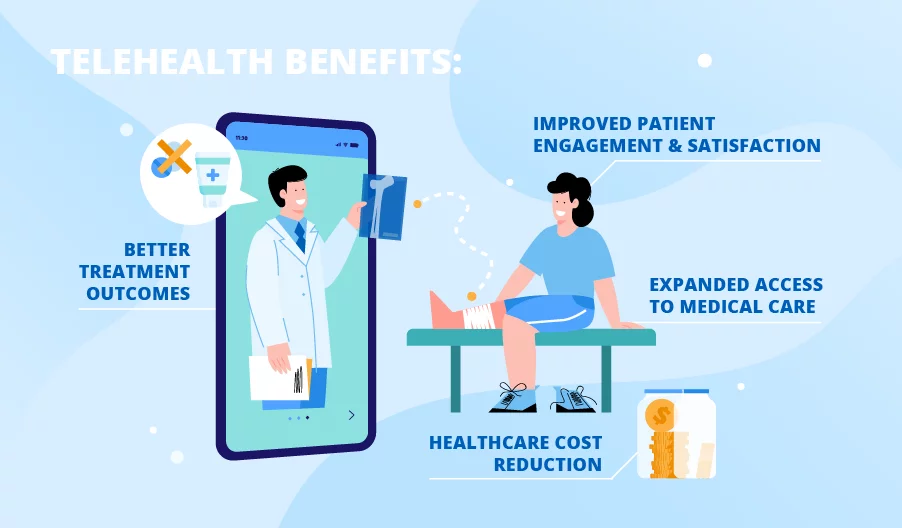
When any new concept is introduced in the medical field, it is an evident question for the end consumer to seek that whether this concept could be feasible, effective and well accepted by the society. In case of telemedicine and telehealth there have been a lot of studies in order to evaluate its effectiveness and accessibility and acceptability. In doing so, many studies have proven to be in favor of this new technology while many other studies claim otherwise in terms of ethical, monetary and security issues (Cornford & Klecun-Dabrowska, 2001). Telemedicine is one of many ways to use the benefits of Information and communication technology (ICT) (Wootton, 2001). This well-founded coalesce of telecom industry; telehealth and telemedicine seek constant evaluation of the needs of common people and their discretion towards this new found concept (Wernhart et al., 2019).Although telehealth and telemedicine allows a healthcare worker to treat their patients from a distant location, it still keeps the integrity of the holistic healthcare approach rather than focusing on the disease based approach. Albeit these concepts are still in the emerging phase (Darkins et al., 2000) these have introduced the patient care into a digitalized world where face to face interaction of physician and patient is no longer needed. The magnitude of importance of telemedicine and telehealth can inferred from the fact that diabetic care alone cost for $132 billion annually, whilst the use of these updated technological services, not only the cost has decreased over all but also the quality of care has been enhanced too (Brewer et al., 2011). These digital technologies being very cost effective and easy to approach will not only benefit the healthcare providers and the patients, but also the policy makers and the stakeholders as well.
What is Telehealth?
There are three interchanging terminologies being used in the context of remote medicine that are telehealth, telemedicine and e-health (Monteagudo et al., 2014). These are very comprehensive terms that are used in context to information and communication technologies (ICT) in health-related services (Wernhart et al., 2019). The information carrying technology comes in different set ups depending upon the consumer demand for example a single and simple stand-alone database system for a small nursing home while a huge multiple system interorganizational system that organizes and connect different administrative processes (Cornford & Klecun-Dabrowska, 2001). Telehealth is the accoutering of medical facilities from a far via various telecommunication technologies for example telephones, mobile phones, emails, even with or without the need of video calls (Mokdad et al., 2018). This phenomenon was first introduced at about the start of the twentieth century even before the invention of television (Orlando et al., 2019); hence the kind of telehealth we talk about today was a bit different in the beginning. It evolved from being a group therapy sessions, joint sessions of nurses and medical staff members, conventions for educational training and even in some cases the involvement of the physician was not even present (Maheu, 2001). But eventually, with the passage of time, improvement in science and technology and increase in awareness among people, telehealth has taken a new perspective. Telehealth basically falls into three main categories:
Asynchronous communication
In this type of communication the patient related images, confidential files and other patient related esoteric medical information is stored in a feed and then later sent to the physician when required. The physician then sends his appropriate assessment results back to the patient (Sikka et al., 2014).
Remote monitoring
This is a type of telehealth usage in which the patient information is fed in a central monitor; extracting readings from the sensors ad telemetry devices attached to the patients located a far (Sikka et al., 2014).
Real-time of synchronous communication
It is a kind of telehealth and telemedicine in which doctors and other healthcare providers are in constant interaction with their patients via a real-time telecommunication device such as a telemetry or videoconferencing (Sikka et al., 2014).
There are many advantages of telehealth with respect to time, money, knowledge and quality such as: reducing the travel load of patients, accelerate and ease the access of healthcare facilities regarding the appointments, medicine prescriptions and rescheduling, and improves the end user expectations (Tuckson et al., 2017). With the help of telehealth, many nurses and doctors are able to examine and monitor their patients from a far such as screening their blood pressure, ventilation rate, heart rate, oxygen saturation and temperature. These readings are then sent to clinical review via the broadband services (Taylor et al., 2015). This not only saves time of the patients and as well as of the doctors but also saves the travelling cost of both parties.
Nowadays, various means for using telehealth, like telephone, mobile phone, or even smartphones can be used to connect to our physician and take guidance in any emergency situation, take a second opinion regarding any major decision or take suggestions regarding any change of medications and other patiently routines (Darkins et al., 2000). It is a constantly evolving field of healthcare that is breaking the status quo of traditional medicine and healthcare delivery systems, where face to face interaction of the patient and the caregiver was necessary. The world wide acceptance and normalization of this advancing medical technology can be inferred by the fact that majority of the patients have yielded a very positive response and a high level of satisfaction from using this means of healthcare delivery (Polinski et al., 2016). They found this concept very cost effective, enhanced outcome, time saving, easy to use and they felt an improved patient-doctor communication (Kruse et al., 2017).
What is Telemedicine?
The rapid advancement in Information and communication technology (ICT) left its strong image on the medical field as well, hence burgeoning promising technology interfaces like telemedicine, telehealth or e-health. According to (Wootton, 2001), telemedicine has a no proper definition by the book, although the literal meaning that can be inferred is “health [care] at a distance” (Maheu, 2001). Also jot down a definition of telemedicine stating “the provision of healthcare services, clinical information and education over a distance using telecommunication technology that existed long before the internet.” The basic purpose of this incentive is to deliver healthcare services to people living places with terrain barriers and dispense basic medical services like assessment, diagnoses, and therapeutic care facilities (Evans et al., 2018).
In addition to providing health care facilities from a distance, telemedicine also
- eases one’s ability to reach for healthcare while being cost effective at the same time (Jenkins & McSweeney, 2001)
- improves the quality of healthcare services
- a patient can be benefitted from more than one consultant at a time (Wootton, 2001)
- enhances the paucity of healthcare professionals by the means of collaboration and team work and
- Also helps the authorities in enhancing the delivery of public health services and primary care facilities (Wootton, 2001).
Telemedicine is on its way to reach new heights of success the groundwork of which was laid down by the commercial space center named MITAC (Medical Informatics and Technology Applications Consortium) at Yale University in 1977 by National Aeronautics and Space Administration (NASA) (Chellaiyan et al., 2019). Its implementation is still in the primitive phase (Broens TH) and requires a lot of research as well as awareness not only among healthcare professionals of all types but also among common people. In spite of the fact that the demand of long term health care is increasing day by day, normalizing of telehealth and telemedicine and other related technologies still need more time as its use is uncertain and indeterminate among many end users (Taylor et al., 2015).
Historical perspective of telehealth and telemedicine
When we talk about the terms ‘telehealth’ and ‘telemedicine’ we consider the usage of modern ways of communication like telephone, television, smart phones, video calls etc. But seldom do we know that many years ago when these technologies were not even invented, people were still able to convey their messages to each other. For example, when the bubonic plague started to spread among human beings, people started to mount yellow flags on their ships to demonstrate to others that their ship is having isolated people. Similarly, when it reached a village in U.K. people raised flags and sign boards over their houses to let other people know they have a bubonic infected patient (Darkins et al., 2000).
Studies have it, that telemedicine has been a part of our lives from the first half of the 20th century when electrocardiogram used to be transferred over the telephone lines. Later it played a very important part during the natural calamities in Mexico and America in 1985-88 (Chellaiyan et al., 2019). In retrospective, the use of telemedicine and telehealth eventually wore off in these past years, mainly because of the reason that the telecom industry was expensive at the time and the quality of the images and other virtual means was not up to the mark. Moreover, the acceptance and affiliation of virtual healthcare delivery was not normalized by the general people as well as the doctors themselves (Darkins et al., 2000).
Telehealth and Healthcare providers
Telehealth and telemedicine have been a great source of help and ease for all healthcare professionals starting from physicians to nurses. These technologies and services have not only become an imperative part of the patient’s assimilation of healthcare but have also helped healthcare providers to communicate and consult with each other more effectively (Tuckson et al., 2017).
Telehealth and Physicians
The normality of telehealth and telemedicine depends partially on the doctoral community as well as the patients. One of the five main factors by (Monteagudo et al., 2014) discussed earlier, the acceptance of this new norm by healthcare providers play a major role in propagation of this concept. Telehealth has aided clinician to clinician communication in various fields such as dermatology, radiology, surgery and emergency and ICU (Tuckson et al., 2017). There are able to discuss complex scenarios with each other and also consultation from other medical expertise is also made easy. Doctors are able to look after their patients with chronic disabilities and ailments, management of medications is easy, they can assist in wound care, counsel them whenever needed and most importantly they are able to track their patient’s health after their discharge from the hospital. Telehealth improves coordination between different healthcare professionals and give them access to acquire elemental medical skills from other specialty and help them in keeping up with the attest upgrade in the medical field. It has been stated in a paper that “E-medicine is the use of information technology including the internet to develop and implement new models for the business and clinical processes f or health care. (Center for Total Access, Fort Gordon, GA, www.cta.ha.osd.mil)” (Whitlock et al., 2000).
Telehealth and Nurses
In order to meet the increased demand regarding the necessitation of healthcare services, Telemedicine and telehealth have been a source of relief and a great help for all community health nurses and advanced practice nurses (Jenkins & McSweeney, 2001). A study conducted in one of the states of America that about one fifth of the nursing community worked had the employment in the telehealth industry (Charles, 2000). This clearly shows that the concept of telehealth and telemedicine is becoming popular in the nursing community as well and people are taking advantage of this benefitting service. Telecommunication services are been taken into account in the nursing department slowly and steadily with nurses facing the challenges on how to integrate this new technology in order to lessen their workload and understand how this will implicate on their patient’s health care delivery (Taylor et al., 2015). It is therefore suggested to improve and recuperate the nursing curriculum and train the nurses to deliver an ethic-friendly and profound telehealth and virtual care. Nursing staff has been an active user of telehealth services by triaging patients according to their severity of disease, need of care and sending them to the appropriate department of care via a telephonic interview (Rutenberg & Oberle, 2008). Although this kind of triaging can lead to healthcare disparities and other ethical issues, it is still under the shade of further research.
Telehealth and patient safety and satisfaction
People have accepted to a much greater extent the concept of this cost effective and easy to approach known as telemedicine and telehealth. Not only do they prefer this method of patient-doctor interaction but also they encourage and support this means of communication. but as a matter of fact, patient satisfaction and contentment had been and still is, the biggest concern of healthcare organizations (LaMonte et al., 2003). Not only patients but the physicians and doctors have also been reported to have a say of ‘highly satisfied’ in terms of high quality healthcare delivery, physician to physician collaboration, mentoring and learning perspectives. Doctors have been taking advantage of this extremely efficient technology in many medical specialties such as dermatology, cancer care, primary care, rehab care, ER services, surgery, pediatrics, mental disorders, obstetrics etc. (Sable et al., 2009). Moreover, this technology is also been considered highly safe in terms of telediagnosis, telehomecare and telepharmacy yet a lot of research is required to further evaluate the safety protocols of telehealth and telemedicine (Monteagudo et al., 2014). People living in remote and distant areas although are highly satisfied by this mode of healthcare delivery system as it saves them the extra commute time and provides them with high quality healthcare, there are still speculations among the researchers that the exact definition of satisfaction is not yet provided hence the literature needs more time and research to validate this fact (Orlando et al., 2019).
Future implications of telehealth and telemedicine
According to (Gunderman, 2014), the factors that would play a huge role in the future administration of telehealth and telemedicine are the technology, acceptance, financing, organization and policy and legislation. Acceptance of this new norm bit the healthcare providers and the common people both will help in spreading the awareness of benefits of using this way of healthcare delivery. At the same time, financing from the authorities is as equal as the normalizing the use of technology. The conventionality of telemedicine reached its peak in America in the years 1994-95 when the federal government allocated a budget of around 100 million dollars for it (Maheu, 2001). This clearly shows the importance and need for a reasonable budget to be allocated for this concept to be used normally. Because latest technology is expensive and not every tertiary care hospital can afford the expense. Thus, an idealistic state of mind is required from the multidisciplinary authorities to make policies and laws that are beneficial for both the health care providers and patients for using telehealth facilities.
There are many ways in order to increase the popularity of telehealth and telemedicine and there are various ways to convince the general population to in cooperate this way of healthcare delivery in their lives. WHO has incorporated many organizations in different countries of the world in order to evaluate the percentage of different interdisciplinary fields of medicine that are taking advantage of telehealth services. Continuous inventions in the end user technology market (introducing more high technology gadgets, biosensors, ultra HD video and image capturing devices etc.) in order to attract monetary capital for the expansion and growth of the product. Contraptions that are easy wear and easy to use and have high definition functionality can help in proliferating the concept of telemedicine (Tuckson et al., 2017). Additionally, advancement in telecommunication services such as introducing 4G and 5G services will increase the quality of imaging data transfer among the first and the end user both. Telemedicine and telehealth are paving their way in different medical fields starting from dermatology, emergency medicine, palliative care, neurology, and even in surgery (Evans et al., 2018). There are organizations like the American Telemedicine Association, that are at the disposal of amalgamating different groups such as academia, medicine, telecom technological companies, allied health care providers, and other government officials, for continual formulations and revision of the guidelines that are necessary for an effective healthcare delivery via telemedicine and telehealth (Cucoranu et al., 2014). With the advancement in medical and telecommunication technology, the interdisciplinary care is taking full advantage of this opportunity, the details of which will be discussed later in this paper.
Difference between Telehealth and Telemedicine
The international forum that is responsible for the healthcare policies worldwide distinguishes the difference between telehealth and telemedicine as “If telehealth is understood to mean the integration of telecommunications systems into the practice of protecting and promoting health, while telemedicine is the incorporation of these systems into curative medicine, then it must be acknowledged that telehealth corresponds more closely to the international activities of WHO in the field of public health. It covers education for health, public and community health, health systems development and epidemiology, whereas telemedicine is oriented more towards the clinical aspects’’ (Darkins et al., 2000). In context of the syllables in the word ‘Telemedicine’, tele is borrowed from the Greek language, which literally means ‘distant,’ which means practicing medicine from a distance. Whereas on the other hand, health means free from any disease or illness, ultimately giving a whole new meaning to the concept of telemedicine.
Telehealth is the amalgamation of telecommunication and the medical services for the purpose of delivering and promoting healthcare services while telemedicine on the other hand is the use of these services for the curative medicine. It describes a more wide range of healthcare services that goes beyond the clinical set ups into the homes of the patients and the communities and using an extended range of technologies ranging from internet, internet, online websites to audio and video calls and online chat sessions (Cornford & Klecun-Dabrowska, 2001). It includes the patients of all age groups ranging from children to young adults and to the geriatric population. Telemedicine is an umbrella term that is specifically used when addressing the delivery of all sorts of therapeutic interventions of the underlying diseases. But as we move forward with enhancing technology and broadened frame of mind, we prefer that the use of this concept should not be restricted only to curative medical interventions. End users of healthcare services are contracting services that range from health and disease prevention, secondary intervention that include therapeutic care through to palliative care. Hence there was a need to expand the horizon of telemedicine and include under the umbrella other healthcare facilities other than just the medicinal care. This is the reason the term ‘telehealth’ was coined that deals with all sorts of medical facilities like assessment, diagnosis, imaging, therapeutic facilities, rehab, emergency care and consultation purposes. Moreover, it is also being used within the doctoral and other healthcare providing community for learning and mentoring purposes (Evans et al., 2018). Physicians and doctors use videoconferencing and telecommunication services to arrange seminars, conferences and webinars in order to educate their peers and discuss complex cases and assist each other in unusual situations. For example, if there is a webinar that is needed to be conducted and the participants are in different countries at the moment, the this could be easily be arranged with the help of using the tool of videoconferencing no matter how distant the other end participant is. Whereas telemedicine deals with the delivery of curative facilities to the patients it does not include any clinician to clinician to interaction for any sort or purpose. Telemedicine is considered to be limited when we talk about the smoothness of doctor-patient interaction (Maheu, 2001).
Telehealth is a terminology that is often replaced and/or is a substitutable term for telemedicine (Tuckson et al., 2017). Telehealth is a much broader term under which we can substantiate the term telemedicine and if the purpose of telemedicine is been encompassed under the term telehealth than there is no need left to use the former terminology in literature. There are so many ways and advantages to prefer the term telehealth such as telemedicine only refers to the healthcare delivery that is related to physicians only. Scheduling and rescheduling appointments, medicine prescriptions, and consultations of all sorts. Pragmatically speaking, physicians and clinicians are the key stones when talking about the healthcare delivery and they should mostly be dealing with the patient in the traditional face-to-face manner. With the introduction of the term ‘telehealth’, the role of physicians is being also upgraded as they no longer work as an autonomous body but as a member of an extensive healthcare team. Nevertheless, it would be unfair to use a term that spates one discipline of medicine from the other, whether it might be medicine, nursing, rehab or any other, the intention of delivering team based distant health care would eventually die. With the progress in time, as telemedicine has started to deliver home based health care and also started dealing with awareness programs among the healthcare professionals and the patients as well, it was well thought that it would be fair enough to drop the term telemedicine as it is reaching beyond its concept, and start using a more broader term ‘telehealth’ in the respective context (Darkins et al., 2000).
As this technology has been with us since the past century, there have been so many terminologies that have been in context to this concept. Telemedicine was the first term that was used in terms of addressing the distant healthcare delivery while today quite a few terms have been introduced that are starting to replace the term telemedicine by e-health, telecare, healthinformatic, healthtelematics etc. Telehealth on the other hand is considered more girdling by many authors as compared to telemedicine (Maheu, 2001) as it not only focuses on using technological software for therapeutic purposes only but also for diagnosing, teaching, learning, administrative purposes and examination and assessment as well. It encompasses the primary prevention but also addresses the secondary and tertiary prevention as well (Cornford & Klecun-Dabrowska, 2001). These terms are most of the time interchangeably used in different contexts therefore this variety of jargons are a proof of this field’s expansion and positive growth. Telemedicine and telehealth terminologies although are considered having a different contexture background, yet they are being used interchangeably and their use is however mainly dependent on the perspective of the user. With the upcoming future, it is predicted that the differences between these terminologies will be so minute that it would be inconsiderable (Darkins et al., 2000).
Ethical Challenges and Concerns Regarding Telemedicine and Telehealth
The consumer health informatics has widened its horizon since the start of the 2oth century. These technologies not only provide beneficiary services to the ill population but also provide preventive measures to the healthy and at risk population as well. The propagation of telehealth and telemedicine and its vertical integration into out communities and society has eradicated the circumscription of geographical barriers cultural or any ethnic restrictions in the transfer of healthcare delivery. As a result of this invention the medical facilities have transferred from big tertiary healthcare buildings to homes, community based health programs, audio or video calls and even online chat sessions (Orlando et al., 2019). As much as this has eased our lives but at the same time has opened windows of ethical and privacy concerns with respect to the patient’s data. The increasing trend of using telehealth services in our daily lives and its colossally expanding role in the society has solved so many health related issues and eradicated various healthcare disparities yet at the same time it has aroused questionable circumstances that has led its debatable credibility. Internet is like an open sea. There is tremendous amount of information available on sight just a click away. Doctors and patients both of them are now accessing medical information, new treatment updates and insurance policy data at the same time. As a result of telehealth, well-educated and self-taught patients have now changed the paradigm between the doctor and patient relationship completely. Although this has its own pros and cons, but one of the major pros of this technology is that a well-educated and well informed patient can make the best decision for himself regarding his medical condition.
Ethics have a very important and deontological place in the healthcare and medical field. This word is coined on the basis of the consideration of whether an action or a decision is right or wrong in itself, made with respect to the context of a clinical scenario or in general to say the least (Cornford & Klecun-Dabrowska, 2001). This decision of an action or a deduction being right or wrong is not consequential, but depends on the accordance of the morality scale. Ethics can be defined as ‘about how one “ought” or “ought not” to act based on values’ (Rutenberg & Oberle, 2008). It clarifies the rights of the patients, obligations of the healthcare staff and the need of equating the balance among the different forms of interests (Cornford & Klecun-Dabrowska, 2001).
Online access to healthcare information
With the exponential proliferation of telecommunication technology in the field of medicine, it is equally concerning that the number of ethical issues that arise with it are getting overlooked and no one is talking about it. There are plethora of online websites that have devoted themselves to provide diagnosis, therapeutic plans, risk factors, pathophysiology, risk management, medications and everything related to the diagnosis of a disease till its worst case scenario. All of this information is stored online ready to be availed by consumers. But this ease in the healthcare accessibility is backed up by many concerns. Some of these concerns include the maintenance of the quality of internet-based healthcare delivery, the containment of consumer’s privacy, accessibility to authentic and research backed up authentic healthcare information and the autonomy of what to choose and what not in the sea of enormous information. As the time passes by the inclination towards using internet for self-diagnosis and self-treatment grows exponentially and with it is therefore required to maintain the a secure internet connection where the privacy of the consumer is promised, elevate the quality of authentic content and low cost products for the general population. Hence even in the absence of a healthcare provider, a person can still take medical advice from online sources.
Ethical issues in healthcare setup
Telehealth triage is a system of categorizing, assessing and referring of patients according to the severity and extent of their medical needs with the help of a telephone. Nursing taking part in the telehealth telephonic triage are highly skilled and critical thinkers yet they encounter a number of moral dilemmas, ethical concerns and moral uncertainty. Since nurses do not see their patients in person and they have a designated time in which they have to complete the telephonic interview, there can be a lot of differences generated between the nurse’s believes and that of the patients (Rutenberg & Oberle, 2008). Disparities generated due to these differences may lead to ethical issues among the nursing care staff. In addition to this there are also evidences of language ethical issues among the nursing staff while dealing with their patients through a telehealth service.
Privacy and confidentiality of the patients
Back in the time, all of the patient’s past and present medical information and demographics used to be stored manually, handwritten on papers. It was quite easy for anyone to their hands on the personal information of whosoever they wanted. But then came the Digital Era. In these times all of the patient’s important information is stored on a computer system or software. As the healthcare providers uses ‘store and forward’ technology most of the time, which means that the patient’s past medical history, presenting medical complain, diagnostic imaging and other crucial insurance data is stored within a third party system. This complicated turn of events has led to an increased fear of the data getting hacked by the hackers anytime (Berwick & Gaines, 2018). Patient’s intimate and private information is stored in a third party interface, a software called as ‘store and forward technology’(Eedy & Wootton, 2001), saves patient’s information and then forwards it to the physician or the patient himself when required. This creates a cautionary space where hackers can easily hack the system and all the confidential and private data of the patient can be leaked. Although this software is of great practical use but if given in wrong hands can create a huge mess related to the confidential stuff of the patient.
Ethical concerns beyond privacy and confidentiality
When it comes to using telecommunication technology for medical and healthcare purpose, the ethical issues that are concerning are not only just the privacy of the patient and the confidentiality of his intimate data. The concern goes beyond these two contexts into the effectiveness of relationship between doctor and the patient, accessibility to the healthcare facility, the ability to provide evenhanded medical treatment, cost effectiveness and the effect on the quality of patient’s life. This can be explained by taking the example of a case scenario, if telemonitoring service system is opted instead of hiring a nurse in order to monitor the vitals, medication adherence and overall daily routine of a weak older man in his house. One end of the monitor is connected to the patient in his house while the other is connected to a nursing station in a tertiary care hospital. This method of distant monitoring was appreciated by both the doctors and the [patients as well. For patients it was cost effective, easy to handle and more inclusive while for the doctors this service was less time taking and they did not have to live the hassle of greetings and good byes every day. But one may ask that there are two faces of a coin. The ethical concerns clinging to this ideal case scenario is the long-term consequences of this healthcare delivery, the effect of this readily available yet non-socializing system on the mental health of the patients, foreseeing the future implications on the healthcare provision and professional roles of the healthcare providers (Cornford & Klecun-Dabrowska, 2001).
Telehealth and the right to choose
Ironically when we speak that telehealth and telemedicine are very cost effective technologies that are easily available and readily accessible to everyone especially people living in rural areas that face geographical borders in order to visit a good authentic clinician for an emergency checkup. These rural and underprivileged areas are devoid of such modern technological stuff as the financial status of people living in these areas is just below the belt and they cannot afford to buy these technological devices in the first place. This scenario comes under the umbrella of an unethical claim that instead of building high quality healthcare institutions there instead people living in rural and underdeveloped areas are forced to choose a healthcare plan that utilizes a gadget or an ICT device that is unaffordable for them.
Insurance policies and reimbursement claims
Another ethical that arises with respect to the use of telehealth and telemedicine is the insurance policies and reimbursement claims for the people suing these electronic services. Reimbursements are being provided to all the citizens of rural areas but the point of concernment is that if telehealth has been introduced in such areas than there should be telehealth care policies established to cover these area of people as well (Tuckson et al., 2017). Moreover the accessibility and equity to use these technologies in such underdeveloped and low educated population is plain unfair because these services are acceptable for only those population of people who have dominantly been using these services from the start. A study states that ‘Widespread adoption and use of costly telehealth technologies for mental health services may be limited by low reimbursements for telehealth services’ (Wilson et al., 2017) Although telehealth has a positive implication for the mentally disturbed patients but the reason of this concept being costly and out of reach has led to forgoing of treatment process at all even a face to face traditional way too. Same is the case with the availability of internet services because there are people who either cannot afford the internet facility or there people who prefer not to use internet at all. This ethical concern of improper and unequal distribution of telehealth services is troublesome and needs to be addressed soon hence these facilities should be made available in all rural and backward areas.
Disparities in current healthcare structure which necessitate the need for telehealth and telemedicine
Human beings have constantly been evolving since the day earth came into being. Whenever there is a hole or a gap in a proposed structure, humans tend to fill that gap through thought provoking innovations. Similarly, the field of medicine has been evolving from hundreds of years. Many new innovations and discoveries have been recorded till date. These discoveries had resulted in the answer to the disparities in the practice of that time and the call for a change and improvement. In a similar context, there has been a lot of research going on relating to various disparities in health care in today’s date. There are many discrepancies that call out for an upgrade, if not a complete change, in the healthcare delivery system as we step into a more advanced and digital age. The shift of paradigm from the traditional face-to-face doctor patient consultation to telemedicine and telehealth in the healthcare industry was merely the consequence of this advancement. The need of telemedicine and telehealth to be incorporated into our routine medical grind has is underemphasized. There are a lot of disparities in the current medical practice that call out for the services of telehealth and its maximum integration in our daily lives. The inequity in treating the minority groups of the society (Lyerly et al., 2016), the age and gender disparity, the medical condition disparateness, the cost disparity (Weaver et al., 2010) are few of the many disparities that are being practiced in the medical care community and demand for a new way of healthcare delivery system.
One of the most common healthcare disparateness that influences the use of telehealth and telemedicine is the high cost of the medical facilities. The increased cost of medical establishments, prescription medications and the medical copayments that a patient has to pay to his insurer has led people to forgo the medical treatment they medically require (Weaver et al., 2010). Cost has always been a major concern in the accessibility of the medical care. In today’s date when the monetary value of every object is peaking evidently, there is no age group that has not affected by this situation. There are fewer jobs available in the market so when a student graduates, he is jobless by definition. Similarly, geriatric populations who do not have enough pensions also think twice in order to opt for any medical treatments. Insurance policies have been complicated enough that people not to seek them anymore. Cancer survivors, patients who have been declared cancer free after their respective treatment, have been noted to ignore their further on going treatment regime just because they cost more than their wages. In addition to these medical expenses, the expense of the commute to the healthcare facility also creates a barrier for them to acquire the required medical treatment. In this state of matter, telemedicine and telehealth have proven to be cost effective in more than one ways. Moreover, people with disabilities (Bove et al., 2019), more specifically older age groups, tend to less incline towards seeking medical attention even though they have a medical insurance covered. The disparity of healthcare accessibility is one of the major reasons that are related to increased mortality and morbidity rate among older adults. In addition to this the cost-related hindrances in accessing the medical care only worsens the situation (Bove et al., 2019). Telehealth on the other hand not only provides a cost effective solution to the older population but also provide them with technology that is easy to handle and readily accessible. Especially disparities that older adults with disabilities have to face like structural hindrances, for example, inconvenient physician’s office or unavailable medical facilities in their vicinity, can easily be overcome via the use of telehealth services.
Disparities in mental health delivery have been spiking lately with the experts saying that these discrepancies are of different stature as compared to the others (Aneshensel, 2009). More specifically the ethnic and racial disparities in the mental health delivery have been the hot topic that needs to be addressed. These minority groups have a lesser frequency of hospital visits, low medication adherence, and low inclination towards seeking medical help for their mental problems. Societal pressure and degrading have hindered many mental disease sufferers to avoid visiting clinics for help (Aneshensel, 2009). This has not only led to spike in mental health issues but also increased severity of the problem. Telemedicine and telehealth can help eradicate this disparity by providing a safer environment of patient’s own home while seeking medical advice and therapy sessions. People with depression, anxiety, and other mental disorders who feel uncomfortable in being exposed to the world while visiting a hospital, can attend their therapy sessions via videoconferencing, audio telephonic calls or store and forward technology without getting out of their homes (Charles, 2000). The doctors can either have a direct contact with the patient seeking mental health treatment or he can use telehealth as a monitoring system as well. The lack of comfort between the doctor and the patient can lead to improper and incomplete sharing of medical information that can eventually lead to misinterpretation of diagnosis and ineffective treatment plan. This not only affects the health of the patient but also the morale of the physicians as well. Hence using telehealth as a source of therapy, which usually occurs in group sessions where people with same medical backgrounds and diagnosis come together and share their problems, one can share his past medical history and understand his treatment sessions in a better way (Stamm, 1998).
Figure 2: Accessibility of mental health care facilities among different racial groups in U.S.
An accurate healthcare delivery system depends on two major data sources: the information related to the patient and the medical knowledge of the doctor. The doctor must be able to assimilate the patient information about his medications, past medical history, previous, risk factors and other comorbidities in order to get to a clinical diagnosis and plan a treatment protocol. When doctors and patients come from different cultural backgrounds, it’s difficult for them to create an environment of comfort and trust between them, leading to racial and ethnic disparities. Ethnic and racial differences between doctor and the patients can result in problematic and incomplete examination and treatment interventions (Lyerly et al., 2016). The factor of physician’s uncertainty regarding the patient’s diagnosis or even his treatment can play a huge role in the mistrust and inclination of the patient away from the treatment. Patients who expect racial or ethnic disparity from their physician tend to take his medical advice lightly, if anything seeking medical advice at all. the existence of stereotypes and biases towards a specific group of people or minority by the healthcare providers can create huge disparateness in the healthcare delivery (Richardson et al., 2003). Telemedicine and telehealth facilities tend to eradicate this trend. Statistics have shown that the highest number of acute stroke cases have been reported among the minorities in the USA hence leading to disparities in accessing the healthcare facilities (Lyerly et al., 2016). Studies provide evidence that once the minorities develop symptoms of acute stroke and they reach the hospital, they have to wait longer times in order to get the gold standard treatment, the tissue plasminogen activator, hence increasing the mortality and morbidity rate among them (LaMonte et al., 2003). Telemedicine not only provides a saver environment for them at their homes but also a guaranteed and on time treatment for them (Wechsler et al., 2017). Telemedicine and telehealth services not only provide neurological expert services to small working hospitals for minorities but also bridges the gap of ethnic and racial disparity in the access to the acute stroke treatment (Lyerly et al., 2016).
Minority groups face a lot of risk factors that contribute to their increased mortality and morbidity rate. Low financial status, low social status, environmental risk factors, language barrier and their beliefs of health related to their culture. To add more fuel to the fire, health care providers also show biasness while these minority groups for example, making them wait extra-long in the queue to avail medical care (Richardson et al., 2003), giving them inadequate amount of medicine and unfair insurance policies and reimbursement rules (Harris et al., 1997). It has also been noted that Hispanic patients are more likely to get inadequate amount of general anesthesia during a surgery (R. Williams & Williams-Morris, 2000) leading to improper therapeutic outcomes and increased mortality and morbidity rate. All these disparities in the healthcare are not only lead us to question the capabilities of human nature of the doctor but also the steps of the authorities and the society that should be taken to consider the minority groups as the equal parts of our society. The concept of utilizing telemedicine and telehealth recently has been started to eradicate these concerning issues among the minority groups. By using telehealth as the mode of healthcare delivery the cross-cultural interaction has been improved by hiring healthcare professionals with multiple linguistic approaches, availing the option of a third party interpreter to translate the medical concerns and adaption of more standard definitions and treatment protocols the ethnic and racial disparity have started to overcome in the healthcare industry (Brauchli & Oberholzer, 2005). The use services like IPATH technology used in telehealth, flexible enough to make necessary changes according to the end user requirements and come up with the particular region based solutions in order to surmount the language and cultural barriers.
Figure 3: Percentages of different ethnicities with lack of medical care availability and high cost disparity
Lack of healthcare insurance policies in rural areas is another disparity that has motivated the community to include the concept of telehealth in their lives. There are small business set ups and low job salaries in underdeveloped and rural areas leading to a decrease number of health insurance being offered to their employees. Moreover, people in such areas are less educated to have know-how of their rights and ask for a deserving health insurance. People living in rural areas have comparatively fewer choices in the health care plan offered to them as compared to the people living in urban areas. One of the main reason is the low level of education amongst the inhabitants and the other being the unavailability of competent and specialist physicians and preferred therapeutic interventions in that vicinity. Telehealth and telehealth can help in spreading the awareness on the guidelines and basic rights related to medical insurance so that people are educated enough to choose what is best for them. The government of U.S has created an internet based website that provides all sort of detailed information regarding the insurance plans of all kinds (Silverman, 2003). This use of telehealth will help underprivileged community in improving the accessibility to the healthcare facilities and an overall improved healthcare aura. Gender disparities have been one of the greatest concerns in the recent years in the healthcare field. The difference of treatment and medical attention given to males and females is very much evident from the statistics that are available in the research. Gender and health both depend upon each other with the society playing the role of the third party between them. Women tend to live a longer life than men yet suffer from more hectic routine, poorer health conditions and more years of dependency in the form of any disability. Gender differences have been in the acquired medical facilities of inpatient and outpatient department, homecare services and other primary care services (John, 2011)
HIPAA and Telemedicine/Telehealth
The need for security and privacy is a fundamental right of every person in this world. It’s a basic human right which personal information he chooses to share with another person, whether it is health related or not. It has been established form the time of Hippocrates that patients have a full proof right to safe guard their sensitive information and share it with people or healthcare providers only they completely trust. The canon law regarding patient’s medical privacy suggests that no one, even the patient’s physician should have access to his sensitive and confidential information, and the patient should have a complete idea of his information storage whereabouts, should have full authority over obtaining a copy of his information and should be fully authorize to make any changes in them regarding any mistakes (Annas, 2003). Before the formation of HIPAA, there a few set of rules implicated by the federal and state governments regarding the data security of patients but due to their ambiguity and uncertainty it was hence decided to develop a more adamant and solid set of rules to protect the sensitive patient data. With the increase in electronic usage of data transferring between doctors, nurses, pharmacists and other healthcare professionals, the need for more strong and reliable security system was needed (Currie & Madrian, 1999).
HIPAA that stands for Health Insurance Portability and Accountability Act was first documented and implicated from 21st August, 1996. It was a law that was passed by the federal government of the United States of America to ensure the security and secrecy of the medical and personal information of the patients acquiring various healthcare facilities through a hospital, home care or any another means. HIPAA consists of five sections that are entitled as ‘Titles’ which provide more than security, portability and privacy of general public’s medical and personal information (Moore & Frye, 2019). Contemporary amendments in HIPAA have made the rules and regulations more accurate and precise and improve standards and have widened the horizons for who must be accustomed to it. The first title of the Act describes the rules and regulations that govern the competency to shift and/or continue the use of medical facilities by the American workers and their families when they lose or change their jobs. The second title has a streamlined directorial provision by stating that the U.S. department of Health and Human Services (DHHS) to develop an archetype for all sorts of e-healthcare transactions and national identifiers for their workers. Moreover, it also contends to the confidentiality of their worker’s healthcare data and averting healthcare fraud and abuse. The third title demonstrates changes in the laws regarding the medical insurance and reimbursements, while the fourth title specifies guidelines for the people having a precedent health condition and has a participation in a group health plan. The last title provides a prerequisite for the health insurance companies and the migrant community of the United States of America (Moore & Frye, 2019). These rules and regulations have been developed to maintain and ensure a balanced security related conditions regarding the confidential and private medical businesses of patients.
Addressing the confidentiality and privacy of medical records of people has been a very crucial and sensitive topic of interest. Every healthcare facility is accustomed to train their employees time to time, which have to deal with the personal and confidential information of their patients, according to the constantly amending rules and regulations of HIPAA Act 1996. Doctors on the other hand are more specifically and routinely trained on the HIPAA rules that deal with the privacy and confidentiality of the patients because they are the ones dealing with the sensitive information first handedly. There are pieces of information that are required to be hidden while at the same time it is essential to disclose some of it in order for healthcare providers to deliver appropriate and efficient healthcare. So it is the duty of HIPAA Act of rules to maintain order between what to share and what not to. Although these regulations are being implicated nowadays more than ever, there are still breaches found in patient’s confidential information. As we step our feet in modern and Digital Age, every person demands of having information at his hands. More so the patients prefer having their reports, medical information, insurance details and other important data in their phones or computer devices. With this aim in mind, the 1996 passage of the Health Insurance Portability and Accountability Act (HIPAA), changes made by the Health Information Technology for Economic and Clinical Health Act (HITECH), and the current 21st Century Cures Act (Cures) has committed to provide these easy to handle medical information to the general public in a most cost effective way possible (Zhao et al., 2019). But the more the information is put out in the internet or on computer software the more there is danger of getting attacked by the cybercrime.
Telemedicine security issues are authentic and require a serious span of attention towards them. As we enter a more digital age, the technological market has introduced new ways for storing data such as the cloud based healthcare services have launched their unmatchable security promises. Consumers can have this cost effective facility with quotidian access and high scalability (Joshi et al., 2016). These storage systems although efficient and suitable, they come with disadvantages of their own. This informational software is at the verge of getting hacked at any time (Donald M. Berwick, 2018). The Heath Insurance Portability and Accountability Act (HIPAA). Telestroke services and Telestroke network urge in strong compliance to the HIPAA instructions while delivering a remote healthcare in case of an acute stroke. If the patient is residing in an another country then the laws and regulations of that country be taken into account and the confidentiality and privacy of the patient should not be compromised (Wechsler et al., 2017). There are different modes of telecommunication that are being used for the purpose of telemedicine and telehealth. Videoconferencing via software like Skype, face time, Whats app etc. But some of the software like Skype are non-compliant with the HIPAA rules and regulations hence all the data that is shared on that medium is not highly protected and completely secured (Almathami et al., 2020).
The security of patient data and its confidentiality has always been a number one priority of telehealth services but with the upgraded information and communication technology and the electronic devices with the usage of smartphones, wireless internet services and wireless networks has made the scenario of security more complex and complicated. The rise in data security is mainly due to the shared wireless devices and networks as well as using public network system. Patient’s important and intimate and private information is stored in a third party interface, a software called as ‘store and forward technology’ (Eedy & Wootton, 2001), saves patient’s information and then forwards it to the physician or the patient himself when required. This technology is present in the mobile phones and gets processed in apps and the provider can transfer to and from these apps wherever and whenever and to whosoever he wants.
This creates a cautionary space where hackers can easily hack the system and all the confidential and private data of the patient can be leaked. The American Telemedicine Association has provided a detailed and authentic protocol in accordance to the Health Insurance Portability and Accountability Act (HIPAA) and must be practiced while using the synchronous data sharing between the patient and the physician. The guidelines suggest that the audio or the video calls during the synchronous data transfer will be secured as “protected health information shall be secured through use of a private, point to-point circuit, Integrated Services Digital Network, Advanced Encryption Standard (AES) 5 encryption, or virtual private network (VPN) for Internet transmissions”. In addition to these security measures, HIPAA has also issued a bit size encryption for the commercial based companies to synchronize with the same bit size to ensure data privacy and smooth fluidity of the system. For example HIPAA has issued a 128-bit encryption for the protection of electronic data whereas the very famous Skype uses 256-bit AES.
Communication barriers with telehealth and telemedicine
The basic concept behind “TELE communication” and “TELE health” is the use of telecommunication technologies and other distance eradicating communication systems and software that help in connecting the two end parties. If there is a default in the telecommunication devices in use or if the speed of the network is not up to the mark then the whole point of using this concept goes in vain. In addition to the faulty network or technological devices, there might be a default in the end user or the healthcare provider using these services. Sometime lack of communication skills, body language adjustment and decoding, time management, self-preferences and acceptance and understanding the cross-cultural limitations can create barriers while communicating with the physician or the patient. If we are to incorporate such advanced and high end technology into our daily lives than the ground work for developing them should be strong enough to build an authentic and reliable platform. In addition to these digitalized hindrances that telemedicine might face, there are other practical implication barriers like the licensing issues, reimbursement of patients, cost of the technology, availability of the technology to every person and many others shall be discussed in the forthcoming paragraphs.
Licensing
Every health care worker whether a doctor, a physician, a nurse, a technologist or any other healthcare professional, it is mandatory for everyone to get their working license before starting their practice (McKimm et al., 2013). Without a license they are not allowed by the law to pursue their medical practice anywhere. This ensures a safe, effective and equal healthcare delivery to all of the patients regardless of their background. One of the most prominent barriers of telerobotics and tetesurgery is the approbation from the administrative authorities and the licensing of physicians (Evans et al., 2018). The state based licensure system was developed in the start of the 20th century and with the advancement in the healthcare delivery modes, this licensure is what restricting the growth of telemedicine and telehealth. The healthcare professionals dealing in telemedicine and telehealth have to communicate with all sorts patients living in different parts of the world or different cities of the country. Therefore, there is a requirement of a national level based licensing system so that the healthcare professionals all follow the same set of instructions and guidelines (Jacobson & Selvin, 2000).
Network and technological inconsistency
Bad network is one of the most pertinent and troublesome issue in context of telehealth and telemedicine. As the whole ground work and baseline of the concept of telemedicine is based on network connection, high quality advancements and availability to all general population is required. A lot of researchers have found out that an extended quiescence period may decrease the quality and efficiency of data transfer n reduce the operator performance as quiescence extended from 1-2 seconds can make telesurgery non-realistic (Evans et al., 2018). Similarly, in the case of teleophthalmology, the quality of the picture is the main core of accurate examination and if the quality of the images is not up to the mark than the whole point of using telemedicine dies. Online electronic consultation is a vital component of telehealth and telemedicine which enables the consumers to get in touch with their primary healthcare providers via information and communication technology devices (ICTs) (Stamm, 1998). Synchronous telemedicine health services that are constantly being used in homecare set ups require constant high quality network connection in order to provide uninterrupted real-time video connection. If the network connection is not strong enough to maintain the link between the two parties then the point of using telemedicine is of no use. Poor audio and video qualities also serve as a very important barrier regarding the smooth run of telemedicine consultation (Evans et al., 2018). Accessibility to a powerful internet source and poor signals availability are one of the barriers in distant and rural areas. People in urban areas can easily get their hands on the wireless connections and devices whereas people living in rural and underprivileged areas find it difficult to get access to them (Bove et al., 2019).
Lack of body language and trust
Telecommunication initially started through telephone and phonic consultations. Even today majority of the people and doctoral community communicate with each other with the help of their phones and audio calls. One of the limitations of this kind of telecommunication services is that both of the parties are unable to look at the body languages of each other. When a patient visits a physician’s office, the first thing that he notices is his overt behavior. This technique of observing the body language solves half of the examination mystery. But in telephonic conversations or digital sharing of data this technique is absent. Moreover, not every physician is good at their conversation skills. This can serve as a major drawback when dealing with patients only through verbal talks (Almathami et al., 2020). This barrier can be overcome by the use of videoconferencing preference but if this mode of telecommunication is not available in some areas than it can be troublesome for many clinicians working from a distance. Telemedicine is frequently been used to bridge the gap between the cross-cultural medical care delivery but the lack of trust due to the absence of face to face contact with the physician and acceptability of the telemedia services between the doctor and the patient may lead to manipulation of the medical history and other important patiently details. This will eventually lead to faulty diagnosis and uncertain therapeutic interventions, all in all an improper healthcare delivery to the patients (Charles, 2000).
Telecommunication services
Albeit the notion of telemedicine and telehealth have been in use for the past 40 years but its practicality by the doctors and the hospital authorities still face many hindrances regarding the cost, patient’s confidentiality, funding policies and an authentic administration for setting up a telehealth network. It is an undeniable fact that telemedicine has provided an innovative way to bridge the gap between high end state of the art medical services and the rural and underprivileged community. People living in rural areas that are underprivileged in many ways do not have the opportunity to own any sort of technological device. Moreover, if these services and devices if still available in such areas, their cost is high enough for them not buy these gadgets (Almathami et al., 2020). These issues not only does create communication barriers between patients and their clinicians but also create ethnic and legal issues as well (Lyerly et al., 2016).
Scheduling conflicts
Another barrier to the communication process during the use of telemedicine and telehealth is the conflicting schedule systems. Loss of internet access or any mishap or default in the devices or telecom gadgets can lead to the mishandling of the scheduled appointments. If the interfacing devices like the phones, computers, internet services, bio sensing gadgets or any other telecom tools, are not working properly then the whole point of telemedicine fades away. Moreover, sometimes there is a glitch in the system that creates a timeline difference between the two parties. For example, it has already been established that telehealth is used for patients with geographical barriers (Wernhart et al., 2019), suppose if the clinician is in a country with a completely different time zone than that of the patient, the scheduling timing of one patient can coincide with the schedule time of another patient from the same country. This can create a definite barrier between the physician and the patient to communicate with one another.
Technological hindrances
Telemedicine has been shown to be a very effective diagnosing and treatment tool for patients who are located at a distant location or locations with geographical barriers (McDonald et al., 2014). These underprivileged and underdeveloped places that have constrained resources might not have the best staff and the latest technology providers or latest gadgets and devices. This can lead to a conflict between the connections of the end users because a physician might be using a high end state of the art telecommunication technology while at the other end the technology is use is not up to the mark. Lack of synchronization between the user capabilities and the capabilities of the technology in use is a considerable barrier in the field of telemedicine and telehealth (Paul et al., 1999). Moreover, underdeveloped systems and less education about using the systems that are associated with telemedicine and telehealth are the barriers are starting to get minimized due to increase in the awareness and advancing field of computer science. Just a few years ago when the network providers were not advanced enough to provide a secure, authentic and strong network connection with the other party. But today with the introduction of the 5G network system, ultra high definition video calls and audio calls can easily be shared even across the borders. In addition to this, heavy data imaging files and past medical history files of the patient can also be readily shared with this high speed broadband power.
Patient related barriers
Patients acquiring the services of Home Online Health Consultations (HOHC) feel exposed and uncomfortable in sharing their medical condition in front of their family members (Almathami et al., 2020). As it is quite usual that the conversation of the patient and his doctor can be overheard by one or many family members in the house, this restricts the patient to open up comfortably in front of their doctors and be completely honest about their medical condition and current health leading to incomplete examination and improper diagnosis which will eventually lead to ineffective treatment plan. Hence, it serves as one of the major communication barrier while using telemedicine for patients in distant areas. Older patients who do not have any idea how to operate such advanced technology serve as a resistance to use fully avail the advantages of telemedicine. Another context to patient related communication barriers is that patients condition of health could not allow him to communicate efficiently, for example, a person suffering from chronic stroke or facial palsy or Bell’s palsy, might find it extremely difficult to effectively communicate and express their emotions and complaints with the physicians on a telephonic connection (Kruse et al., 2017).
Cultural barriers
Telemedicine and telehealth allows a doctor or any healthcare provider to deal with patients all across the world. This in itself raises a question that is the health care providers qualified enough to tackle the racial, cultural and ethnic disparities all over the world? (Lyerly et al., 2016)The relationship between a doctor and a patient is of trust and hope and this only develops after a good communication. And key to a good communication is to understand the cultural and ethical background of the other person. As health care providers have to deal with patients with all kinds of racial and ethnic backgrounds, it is nearly impossible for them to adapt to such a vast spectrum of cultures. The lack of cultural and cross cultural competency is one of the troublesome barriers of telemedicine and telehealth on which the authorities are currently working on (John, 2011).
Figure 4: Barriers in the smooth flow of telehealth in the society
Benefits of integrating telehealth and telemedicine for interdisciplinary care
Telehealth and telemedicine has been accepted in various specializations of medical field. Doctors have been taking advantage of this extremely efficient technology in many medical specialties such as dermatology (Peracca et al., 2019), radiology (Gunderman, 2014), cancer care (Weaver et al., 2010), primary care, rehab care, ER services (Richardson et al., 2003), surgery, pediatrics, mental disorders (Stamm, 1998), obstetrics etc.(John, 2011) This concept is a globally recognized phenomenon and is rapidly being accepted by various subspecialties of medicine. In this research paper a few of the discipline shall be discussed such as teledermatology, teleradiology, teletrauma, Telestroke, Telepathology, telerobotic surgeries, and medical subspecialties including ophthalmology, endocrinology and psychiatry.
Tele-dermatology
The field of dermatology has also gained many benefits in the context of telehealth and telemedicine, more prominent being the military services in the U.S. (Peracca et al., 2019). Soldiers with mostly with cosmetic complaints can get beneficial results while still being on the duty ground. People with various skin conditions can consult with their dermatologists sitting a far without any hindrances. (Taylor et al., 2015) shares positive experience on managing patients with skin disorders via telemedicine. Easy assessment with the help of either real-time video facility or with the help of sharing real time images can help in accurate assessment and hence a better therapeutic outcome. The two very advantageous ways that can used for this purpose are ‘store and forward’ and ‘real-time videoconferencing’ (Wong & Colven, 2019). Store and forward technology means that patients send their affected part’s images and their medical history documents to the clinician via a third party interface and this stored information is retrieved by the respected healthcare provider whenever required. Although teledermatology is gaining its worth of popularity with the coming times, there are still many challenges that are needed to be handled such as its maintainability in different cultural and ethical norms and issues in the legal context (Eedy & Wootton, 2001).
Teleradiology
Teleradiology is one of the oldest users of telecommunication services in the history of medicine. Patients undergoing diagnostic tests like X rays, MRIs or any CT scan, they imaging were then sent to a computer operated by the diagnostician and then at the end it is send to their physician for further assessment. A teleradiology image processing system is supposed to take in, proceed and deliver the radiology read requests and the digital radiology images are then exposed in this system (Gunderman, 2014)One of the incarnations of teleradiology suggest that a radiology processing system is composed of operating components that are supposed to receive radiological imaging data from the from the technologist at one end, extract the useful and required information from it and then pass on the relevant radiological images and scans to the diagnostician at the other end (Cucoranu et al., 2014). Teleradiology has been proved to be a lifesaving technology for acute telestroke interventions as early diagnosis of ischemic and hemorrhagic stroke can be extremely beneficial for the patients (LaMonte et al., 2003). This technology is doing wonders in the low and middle income countries as there are shortages of radiologists there and if there are enough of them, the citizens are unable to afford them. Radiologists in the high-income countries have volunteered themselves through telemedicine and teleradiology to serve in those countries therefore contributing to improve the global health overall. This concept has emerged to be called as ‘humanitarian teleradiology’ (Mendel et al., 2019). As the world is evolving with each passing day and there are innovations in telecommunication technology as well as new discoveries in the field of artificial intelligence, teleradiology will continue to prosper in the coming years not only in high income countries but specially in the low and middle income countries around the globe.
Teletrauma
Trauma is a condition that is inevitable and people should be ready in order to face such situations. With the passage of time the needs and wants of people have become very modern and up to date and hence the technologists have determined to advance the software and shift the paradigm towards digitalization. Similarly, telemedicine has also adapted to this evolution in the form of “teletrauma” and now is composed of different modalities and instruments that not only come helpful pre hospitalization phase but also in hospital and post hospital rehabilitation phase as well. For example, in an emergency situation of stroke when people call at the emergency helpline 911 and thus there is a dispatch of an EMS team for help with a portable CT scan that will help in early assessment of hemorrhagic or ischemic stroke, ultimately improving the quality of outcome (Lyerly et al., 2016). This is teletrauma in a pre-hospital setting. In rural and underprivileged communities where on the spot trauma centers are unavailable and emergency services are scarce telemedicine and teletruama play a vital role in such situations (Bjorn, 2012). The modern ambulances are equipped with high quality vital monitoring services and real-time video facilities that are wirelessly attached to a physician’s workstation in a clinic can help in early examination and acute interventions of the patients. The emergency medical technicians (EMTs) have been trained to perform thoracocentesis and pericardiocentesis on the spot. This has been a remarkable achievement in saving the lives and declining the mortality rate as a result of trauma. The use of telemedicine a third party interface between a local community hospital in a rural area and an urban trauma center can prove to be very beneficial while managing an traumatic patient in a distant location (Kim & Falcone Jr, 2017).
Telestroke
Telestroke is ‘A network of audiovisual communication and computer systems, which provide the foundation for a collaborative, inter-professional care model focusing on acute stroke patients’ (Wechsler et al., 2017). It is a branch of teleneurology that aims at providing distant telemedicine consultations to patients complaining of acute stroke symptoms and other neurovascular conditions. It uses the notion of interactive videoconferencing technologies in order to treat and prevent the acute stroke complications. The main purpose of Telestroke concept is to provide immediate medical services in acute stages of stroke (pre-hospital and hospital stage) but nevertheless, it has been of practice well beyond that time frame, hence the deliver extended services as well ranging from patient’s healthiness, distant survelling of patient’s vitals, primary disease prevention, sub-acute stage of stroke, rehabilitative services (Burkow et al., 2015) and counseling of patients and helping the to rejoin the community phases. This continuously emerging innovative technology (LaMonte et al., 2003) has been introduced to coordinate and facilitate the need for acute stroke management. It consists of group of primary, secondary and tertiary care giving centers that locate the patients and connect them to the provider at the other end. These services are not only available for home care and emergency services but they are also available in different hospital settings and intensive care units (ICUs) where readily available on call stroke physician is not present. In collaboration with teleradiology which is the delivery of radiological images to a distant diagnostician, physicians are able to diagnose the ischemic or hemorrhagic stroke; which is the key to start the acute stroke interventions (Solenski, 2018). In addition to these positive outcomes of Telestroke, there is still a requirement of professional training of all the healthcare professionals, emergency medical staff, radiologists and technologists, to properly deliver the healthcare without any hindrances. They should adapt to the continuously changing Telestroke management guidelines and adhere to them during their job (Lyerly et al., 2016)
Telepathology
Telepathology is the ability to determine the end product of any surgical pathology cases that are located at a distance. This can be done either via videoconferencing or real-time imaging or with the help of store and forward technology. The American Telemedicine Association has given a definition of telepathology as: “A form of communication between medical professionals that includes the transmission of pathology images and associated clinical information for the purpose of various clinical applications including, but not limited to, primary diagnoses, rapid cytology interpretation, intraoperative and second opinion consultations, ancillary study review, archiving, and quality activities” (Pantanowitz et al., 2014). it has proven to be very useful in geographical areas like Africa, where there are shortages of pathologists and the disease outcome has been greatly influenced by the high end professional diagnosis (Farahani et al., 2016). In addition to these positive consequences of Telepathology, there are some limitations attached to it. The main aim of Telepathology is to equalize the outcomes of remote technologies with the gold standard medical imaging technology. But this is arduous in a way that a robotic interface is required between the imaging device and the pathologist operator (Krupinski et al., 2016). Nevertheless, Telepathology has overcome many hurdles that have come across its way and now it is headed towards robotic microscopy, which is now being incorporated to view the whole-slide scanners.
Telerobotic surgeries
Surgical interventions have seen a lot of inventions and concoctions in the past few years. The major milestone achieved in this field of medicine was the minimally invasive surgery or the laparoscopy approach that changed the game of the surgical approach completely. This method lessened the need for the general anesthesia and the consequential pain of post-surgery and it improved the cosmetic outcomes for the patients (Shen et al., 2020). But these positive achievements came at the cost of the ergonomics of the surgeons performing the surgery, the lack of competence among the professionals and lack of depth perception (Evans et al., 2018). These demerits and the advancement in the information and communication technology (ICT) led to an innovative approach towards the robotic surgery. It started from the ground breaker concept of telemonitoring that escalated to telepresence. The idea of telepresence was merged with the concept of delivering medicine at a distant location hence coined the terminology telemedicine. Eventually, this concept was further polished and modernized by the use of robots for the purpose of distant surgeries. Almost all subspecialties of medicine have taken advantage of this highly efficacious mode of healthcare delivery, but urology and gynecology have been benefitted the most (Marescaux et al., 2001) Surgeons are able to perform surgeries from a far with the help of using these advanced telecommunication technologies. This up gradation of minimally invasive surgeries is more specifically called ‘teleoperated robotic surgical system’. This advancement in technology has made surgeons to overcome the limitation of the laparoscopic surgeries. NASA is collaborating with other research institutes to help expand the concept of telerobotics in order to facilitate astronauts in space (Evans et al., 2018). This technology can be used to guide astronauts in space regarding any medical emergency and surgeons from earth can even perform surgical procedures for them in space.
Telemedicine and endocrinology/diabetes
Diabetes is an endocrinological disease that has taken the world by storm. It is the sixth leading cause of death in the United States of America (Ciemins et al., 2011) Not only do the older adult are affected by this chronic condition diagnosed as Diabetes type 2, but also the young population is also contracting the disease genetically diagnosed as Diabetes type 1. People who live in rural and distant areas specifically, who are unable to travel the commute on daily basis just to visit an endocrinologist, find it very difficult to coop with their daily lives and the condition (Gellis et al., 2014) Early diagnosis, acute interventions and control of lipid profile and glucose level can reduce the chances of diabetic exacerbations. Moreover, self-management and control and diabetic preventive care are all part of an effective plan of care for the diabetics. Primary care physicians, nurses, endocrinologists, diabetic specialists all work together in an interdisciplinary team to provide basic healthcare facility and aware the patients of all the risk factors that are related to diabetes. But the shortage of the providers and geographical barriers has led to acceptance and propagation of telehealth and telemedicine especially in distant and rural areas. Telehealth and telemedicine have proved to be very effective in providing diabetic healthcare facilities and awareness to the people in remote areas (Gómez et al., 2002).With the help of this technology, awareness of primary prevention and diabetic risk factors in addition to the treatment of diabetes is efficaciously delivered to the patients of the underdeveloped areas. And the patients have received this technological concoction very well as it is user friendly and cost effective at the same time (Ciemins et al., 2011).
Telepsychiatry
Telepsychiatry is the mode of effectively transferring patient data and receiving educational and therapeutic interventions and counseling via telecommunication services. This mode of counseling has been well received by the general population in terms of clinical application, educational awareness, adding to the research literature and contributing to the field of medicine in general. Telepsychiatry uses the interface of videoconferencing and related modalities in order to deliver high quality psychological counseling to patients located at a distant location (Shore et al., 2006). This form of healthcare delivery is considered practical and satisfactory with having a positive and negative impact on the interpersonal behavior of patients. In earlier times, Telepsychiatry was cancelled due to lack of administrative managements but with the advancement of technology and telecommunication services it has evolved to be an effective solution. Telepsychiatry has been proven to be a partial remedy for this major problem (Hilty et al., 2002). Telepsychiatry majorly falls into four main categories: directorial, informational, and clinical and research. All of these four areas cover the awareness programs, facilitating general population with the necessary therapeutic interventions, managing the technology according to a set of pre-decided models and lastly add to the sea of literature. Remote and rural areas do not have enough psychiatric clinics at their disposal. They either do not have enough education to self-diagnose themselves with any mental disorder or if they do so, they do not have the approach to a well-established psychiatry clinic (Brown, 1998). One limitation that is evident in this perspective is that there is a lack of doctor-patient understanding due to the differences in their cultural background. This can eventually affect the quality of the healthcare outcome. Therefore, it is very much needed for the doctors to understand the cultural background of the patients and frequent communication with them can bridge the socio-cultural gap (John, 2011).
Telehealth and Pandemics
There has been no particular definition of pandemics up until 2009; later on it was defined as ‘epidemic … over a very wide area and usually affecting a large proportion of the population.’ When there is an infectious pandemic covering the whole world, then there is a very less chance of one getting out of the house, even for a regular or an emergency checkup. Taking for example the case of COVID-19 which is the pandemic that spread due to the sneezing droplets of physical human touch (Smith et al., 2020). In these of type of situations it is usually recommended not to go out for any purpose whatsoever. It is situation like these when technologies and advanced telecommunication services come in handy. But it leads us to ponder that telehealth has been used up till now for rural and underprivileged areas or where there were scarcity of high end medical professionals. But today in order to use telehealth as a baseline medical facility, do we really recognize the normality and are used to the handedness f this technology? Do we have enough funds and managerial staff to manage this conventional technology? Telehealth and telemedicine is one of the best ways to deliver healthcare facilities during an infectious pandemic as it decreases the chances of any close contamination due to increased proximity of another human being. Moreover, telehealth efficiently delivers healthcare delivery to lessen the burden of mental depression and stress in a pandemic situation (Stamm, 1998). Any surgical consultations are efficaciously been dealt with the help of telesurgery or telerobotics surgeries amid the pandemic situation (Marescaux et al., 2001).
Teleophthalmology
Ophthalmology is the study of the diseases related to eyes. Telemedicine is spreading its wings in all fields of medicine especially in the subspecialty of ophthalmology. Mostly due to shortage of providers in rural areas or the absenteeism of doctors within the country when they visit other countries for various conferences or seminars, it is that time when patients still can take appointments and issues their issue related to the eyes with their physician. The only limitation to this highly effective mode of healthcare delivery is the slow internet connection or poor connectivity at either ends (Kennedy et al., 2006) diabetic retinopathy is an eye condition that if not treated within the initial time span can lead to partial or complete legal blindness. Telemedicine has played a very important role in the initial screening of patients who had possible diagnosis of diabetic retinopathy. Digital photographs of the patients are shared with the physician via the internet connection and then after proper and complete examination a final diagnosis is made. This method of screening and examining is completely reliable and feasible among majority of the populations. The digital images of the retina are easily shared with the ophthalmologists and the patients and thus an early treatment can be initiated for the diabetic patients. The physicians are able to grade diabetic retinopathy with the help of single fundus retinal digital image (Rachapelle et al., 2013). This facility is a new ray of sun shine for the people living in rural an underprivileged area where physicians are unable to visit due to geographical challenges and busy schedule and the patients on the other hand due to low income and low education are unable to identify tertiary care hospitals and eligible healthcare professionals (Wootton, 2001). This innovative technology not only enables them to get an apt diagnosis but also the physician is able to prescribe their patients state of the art medications as well.
Telecardiology and pulmonary rehab
Pulmonary rehabilitation is an ultimate need for patients having lung conditions like chronic obstructive pulmonary disease (COPD) or asthma. These are mostly arranged in the form of groups and interactive sessions in a tertiary care setting. People living in areas from where either the commute is too long to these places or there is an unavailability of transport to reach these locations, telerehabilitation serves an important means to continue the treatment. A web based, comprehensive multidisciplinary pulmonary rehab programs inside the homely environment of the patients is well accepted by the patients and is proven to be feasible to provide the necessary treatment plan. This method provides an atmosphere that is comfortable for all patients to learn the rehab strategies and ask all the concerned questions from their healthcare provider (Burkow et al., 2015). In addition to this, telecardiology is also at the verge of extreme popularity. The use of videoconferencing for managing the blood pressure, specifically the systolic blood pressure has been proven to be very effective in elderly group of patients who have had a low income source (Gellis et al., 2014).
Telemedicine and Cancer treatment
Cancer is related to severe chronic depression in patients with all age groups. More specifically young adult patients suffer depression throughout their course of cancer treatment. The psychotherapy that is available for most of the patients is held in group forms but this group-session talk can make most of the young adult cancer patients uncomfortable and is undermining for them. With the help of telecommunication and telepsychotherapy, these patients can receive their counseling sessions form the comfortable environment of their homes with excluding the hassle of the road travel as well (Weaver et al., 2010). In addition to seek mental care, cancer survivors are not financially strong enough to afford the long term expensive medications. This leads them to forgo their medical check-ups and reduced adherence to medications. Until now it has been well established that telemedicine and telehealth are cost effective healthcare services, so these healthcare facilities can help these patients in order to see expert medical help within the comfort level of their own homes and also in a very cost effective manner (Weaver et al., 2010).
Improved care for special needs patient group with Telehealth/telemedicine
Special needs patient group require extra attention and care by the healthcare facilitators more than the other patients. They either have a physical disability, for example post stroke, or a mental disability like autism, down syndrome etc. Geriatric population is also being considered as a special need patient group because the care that is required for them is specific and customized. In addition to these, people with cognitive and developmental disabilities also come under the umbrella of special need patient group. These patients could range in age group from young children to older adults and geriatric populations as well. These special need patient groups need enhanced and extra care along with constant monitoring which telehealth can achieve at its best. 24 hour monitoring, group therapy sessions, counseling and a treatment plan that is filled with compassion and understanding encompasses the paradigm of their care.
Telemedicine and children with special health care needs (CSHCN)
Telemedicine and Telehealth is proven very successful in terms of providing special and extra care for patients of all age group having special needs. Not only the patients but also their family members and the members of the interdisciplinary team were highly satisfied by the remote set up program (Hooshmand & Yao, 2017). These extended and revolutionized computing and telecom technology has helped in delivering high quality and efficient healthcare in remote and distant areas that are underprivileged in many aspects. Deserving but underprivileged families that are unable to take their children to upstate tertiary care centers have found a privilege and a blessing in the name of telemedicine and Telehealth. Children with special healthcare needs (CSHCN) in backward areas are one of the greatest consumers of the telemedicine. This technology overcomes the barriers of long route travelling, looking for subspecialty physicians and tertiary health care providers, parents managing their office routines with the appointment timings and the relying on emergency department services or over the counter medications for temporary measures (Marcin et al., 2004). There is no doubt that traditional way of assessing and evaluating the children face-to-face with special care needs is a priority among many patients. However, if we compare both of these methods of receiving health care facilities via telemedicine or the traditional way, then it has been found that majority of the end consumers were highly satisfied with the remote management of their children’s disabilities whereas the health care providers were equally satisfied with the quality of assessment they provided from a far (McConnochie et al., 2015)
Telehealth and childhood depression and anxiety disorders
Depression is one of the most common psychological disorders not only among adults but also among the young adults and children. It is the leading cause of suicide among young adults while it is the most common mental disorder among the geriatric population. Similarly, childhood depression is a very serious matter that needs to be addressed but the professionals more often. This mental issue can be a major cause of short term and long term morbidity among children. Not only does their future is affected as they are unable to coop with their study schedule and eventually lag behind, but their social life is also severely affected. They prefer not to socialize with their friends and family and prefer spending major part of their day inside their room. The most effective treatment to childhood depression is cognitive behavioral therapy (CBT) (Rothbaum et al., 2000). It basically involves in changing and intervening with the unrequired social and behavioral commands with the aim of improving emotional responses among children and enhances their mental coping mechanism in response to any problematic stimuli. At the same time, parents and caregivers are facing difficulty and inability to get access to this facility due to difficult commute, geographical barriers, disesteem towards their child’s condition and shortage of the therapists. At this point of difficulty, telemedicine and Telehealth come to the rescue. Parents and children take full advantage of the sessions from their therapists sitting a far with the help of telecounseling or videoconferencing (Stamm, 1998) With the help of this mode of healthcare delivery, children and their parents attend the counseling session without any hindrances and the therapist is also at his ease to take care of his patient. Both the children and the parents as well as the caregiver very well receive this type of healthcare delivery and majority of the children are found to be symptom free by the end of their sessions (R. Williams & Williams-Morris, 2000). Telemedicine and Telehealth serve as a connecting bridge between the patients who are unable to get access to the primal healthcare facilities and the pertinent health care givers. The whole families of Children with Special Healthcare Needs (CSHCN) have a lot of financial burden as well as societal burden. Using the telemedicine facilities focus on family centered healthcare delivery that not only reduces the financial but also the emotional and mental burden of the families (John, 2011).
Telemedicine and special care need for geriatric population
The geriatric population of our community is increasing exponentially with each passing year. The fertility rate of the world is increasing while at the same time the life expectancy of general population is increasing. The past times, when infectious diseases took a toll and millions and millions of people died in a matter of days. Today these pandemics are contained with the help of newly developed highly efficient vaccines and medicines and the only diseases that are threatening the human kind are the chronic ones. A lot of medications and lifestyle improvements are being implicated in order to syncopate these conditions and curtail them (Gellis et al., 2014). And with advancing medicine and technology the age and health of the elderly is also improving leading to a large percentile of healthy elderly people in the books. At the same time, old aged group of our community needs our full attention and support. They are frail and unemployed hence unable to travel and seek medical attention. Telemedicine and Telehealth very finely address this issue in many innovative ways.
Geriatric issues are complicated. If an older person visits a doctor, chances are that he might be suffering with more than one disease at the same time (Charles, 2000). Usually a person suffering from any cardiac disease is often found to have comorbidities related to kidneys, lungs and peripheral limbs. Older people are more prone to comorbidities as a result of aging process. Thus it is the duty of the primary healthcare facilitator to look up for the complications and be aware of the progression of the diseases their geriatric patient is going through. Telemedicine plays a vital role in this perspective as the primary physician is able to monitor the daily vitals, any positive progressions, any deterioration in health or the need for medication increment or decrement with time, by sitting from a distant place. This saves the older people from the hassle of public commute, saves them lot money and as they are already frail and weak, saves them a lot of energy. For many reasons and under personal preferences, elderly people do not prefer to live with their extended families. They do not have anyone to look after them or report any changes in their health or medications with time. Telemedicine and Telehealth have helped them in ways that is beneficial for them not only in the medical perspective but also emotional perspective as well. Telenursing, which is a subset of Telehealth, has provided the nursing facilities and home care to such elderly without them getting out of their homes. Medication management, compensating the financial issues, psychological counseling and(Gellis et al., 2014) hustle and bustle of travelling are all managed with the wireless healthcare delivery system.
Healthcare providers need to flatten the curve of the older people falling ill as the life expectancy is increasing and the healthcare providers are lessening in number. They can do it by anticipating the crises, limiting the clinic visit, constrain the mental health deterioration and all this doing by respecting the autonomy of their patients and intervening only when it is medically necessary. Shortage of nursing staff, doctors and other healthcare professionals and healthcare nursing homecare main reason telemedicine, telenursing and telehomecare is getting recognition more than ever.
Telehealth and post-stroke disabilities
The rehab of geriatric population post stroke is also a concerning matter of fact. Telerehabilitation is proven very effective in generating a positive response among the training of the assistants, training of the patients for the exercises post rehab, and it is easier for the patients to use home-based technology as compared to visiting the clinics in person. It is also helpful in creating a positive and peaceful state of mind in patients after they are discharged from the hospital and shifted to the homecare facility. There are not many resources ad innovations in delivering a qualitative homecare post stroke rehab, but with the help of telerehabilitation it is a creative and interactive way of encouraging patients and facilitating them in their time of difficulty (Wechsler et al., 2017)
Telemedicine and Autism
Autism is a neurodevelopmental disorder that results in inability to socialize oneself with other human beings, problems and difficulty in verbal and nonverbal speech and constrained behavioral repertoire. The number of children experiencing this condition is increasing each passing year as there is 1 autistic child in a group of every 110 children that shows the signs for the autism spectrum disorders (ASD) (Vismara et al., 2013). There is no proper cure for this condition but an early diagnosis and longitudinal treatment with lifelong rehab is what is required. This crucial situation is getting out of hands as there are not enough trained professionals that can either facilitate autistic children or train their parents or caregivers. This critical situation is covered and eased by the use of telemedicine or Web-based training of both the parents and the children. This not only reduces the workload on the shortened trained professionals but also lessen the burden of autistic families of travelling, finding trained professionals and coping with their own work at the same time (Lindgren et al., 2016). It is because of such reasons that telecounseling sessions are proven to be very effective and result in high end user satisfaction.
Patients with MSK disabilities
Patients with musculoskeletal conditions like multiple sclerosis can also get a lot of advantage from the wireless technology that we call telemedicine and Telehealth. Healthcare professionals are unable to cross the geographical border, can assess their patients and examine the disability level with the help of telemedicine by sitting miles apart. This method has been very effective for patients with mild to moderate Multiple sclerosis (Henderson et al., 2014). Patients with MS are presented with walking disabilities where they either need any assistive devices or proper training to walk or use them. Accelerometers with biosensors are being introduced that not only detect the speed and biomechanics of the patient’s gait but with the help of multimedia and video conferencing, patients can be well trained on how to walk with the help of the assisted devices. This lessens the burden of not only of the families but also saves the extra time and hard work of self-assessment and visiting commute (Bove et al., 2019)
Knee pain is a very common complains among the elderly and in order to avoid its negative consequences on mobility and functional disability, an early assessment and intervention is required. Telecommunication has played a vital role in managing such musculoskeletal conditions without the elderly population getting out of the comfort level of their home. Videoconferencing is found to be very effective in examining the muscular strength and the endurance, the joint mobility, balance and the extent of osteoarthritis of the patients. Moreover this mode of healthcare delivery is also very effective in treating the knee pain as well by teaching different stretching, strengthening and isometric exercises, postural correcting guidelines and balance training. This mode of delivery is well received by the patients as well, strongly agreeing to every aspect of this technology while believing it to be easy to use, less tiring and fun (Zhou & Parmanto, 2019).
Improved healthcare outcomes for chronically ill patients via telehealth/telemedicine
Telehealth and telemedicine have been proven to be of great help when concerning about the acute, primary and secondary health care. This mode of healthcare transmission helps is spreading awareness about a medical condition or a medical treatment and in addition to that also caters the acute medical conditions (LaMonte et al., 2003). But when it comes to dealing with patients who have been suffering from medical conditions from years then the efficacy of telehealth is challenged. Chronic diseases have a high prevalence and are expected to exponentially rise in the foreseeable future hence it is a golden time to provide maximum evidence on a mode of healthcare delivery that is not only easily accessible, cost effective and easy to us (Bashshur et al., 2014). Telehealth provides a better and high quality medical treatment to patients who have been suffering from chronic diseases like cardiovascular conditions (Jenkins & McSweeney, 2001), blood pressure(Ciemins et al., 2011), diabetes (Gómez et al., 2002), musculoskeletal conditions (Bove et al., 2019), neurological conditions (Solenski, 2018) and many others. Telehealth and telemedicine ensure efficacious and potent healthcare delivery to patients with chronic ailments. At the start of the 20th century the major threatening health conditions were the infectious and communicable diseases like Ebola that would wipe out half of the world’s population, but things are changing as we excel higher in the field of medicine and new vaccines and drugs are discovered each year. Today the kind of diseases that pertain human lives are heart disease, endocrinological diseases, neurological diseases, physical and mental disabilities etc. The life expecting of the word is spiking each passing year it is a live evidence that the diseases prevailing amongst the human kind are not the infectious ones but diseases that are entailed for a longer period of time. These diseases do not cause mortality but affect the lifestyle of the people. This is a concerning matter in a way that a large force of healthcare is required in order to manage and maintain an optimal healthcare delivery system.
Chronic illnesses and geriatrics
The life expectancy of human population is increasing (Lyerly et al., 2016), the percentage of older people with chronic diseases in the world is also increasing. The geriatric population with chronic diseases is seen to incline away from using the healthcare facility due to low income and high cost of healthcare facilities even though they are medically insured. Cost related healthcare accessibility is further complicated by the presence of disability in this area of population and the peculiar challenges they have to confront while preceding through healthcare policies. This is the reason why the use of telemedicine is superior to the traditional visits for chronic disease like diabetes, hypertension, pain, congestive heart failure, rehabilitation after stroke, depression, dementia, etc. in older generation (Smith & Gray, 2009). Constant self-management and provident monitoring is essential in managing the chronic illnesses (Piette et al., 2010). This is why telemedicine and telehealth have proven to be very efficient in this field of medicine. With the help of different telemetry systems, audio or video conferencing or different electronic or biosensor gadgets a physician can overlook the changing medical condition of his patients. Even in the underdeveloped countries where people have low income, less education and below the line insurance policy systems, people can still be benefited with this remote technology by using a simple phone calling device (Bove et al., 2019). Telehealth and telemedicine has an advantage of patient inclusion in self-care and self-management of their chronic illnesses, it lets the physicians identify early symptoms of any new onset comorbidity and constraint the aggravation of any present symptoms. Chronically ill population like physically disabled stroke patients, heart failure patients, kidney failure and asthmatic patients, mostly need home based healthcare services and as much as telehealth is boosted to be implicated in such scenario, there is less evidence of its practical implications. As the burden of illness increase with paradoxically advancing technology telehealth is on its verge to serve patients in their homecare settings.
Diabetes
It is the most common chronic illness that has not only affected the geriatric population (diabetes type 2) but also the young adult population (diabetes type 1) as well. According to a report of American Diabetes Association (ADA), approximately 16 million U.S. citizens, or around 6% of the total U.S. population, are probable to have diabetes and a roundabout more than 18% of the older geriatric population has diabetes (Rachapelle et al., 2013). This condition has increased the health related cost and the hospital stay of the patients. Hence telemedicine is found to be efficacious enough to eradicate such disparities in diabetic case management as a study reported “Information technology, through telemedicine, offers the potential for cost-effective, personalized interaction and convenience for both the patient and the provider” (Whitlock et al., 2000). Chronic diabetes always comes with comorbidities such as macular edema, diabetic retinopathy. Although there is less evidence that telehealth can be effectively managed with telehealth, there is a plethora of evidence for early diagnosis, better cost effective and user friendly management of diabetic retinopathy (Rachapelle et al., 2013). Not only does the teleconsultation is accessible for patients diagnosed with diabetes type 2 but home based telecare is also ultra-efficient in declining the numbers of HbA1c and triglyceride levels and inclining the numbers of Low density lipoproteins (LDL) in chronically diagnosed diabetic patients (Whitlock et al., 2000).
Chronic obstructive pulmonary disease (COPD)
COPD is a respiratory airway disease that is the most neglected and undermined of all chronic diseases. Acute exacerbation chronic obstructive disease (AECOPD) is the repetitive occurrence of COPD symptoms and it mostly occurs in patients with last airway instructions and a history of high number of exacerbation episodes in the last year. There have been a maximum number of patient visits in the emergency departments of the hospitals with the complaint of AECOPD making it financially and physically difficult for the patients and their family members to pay excessive emergency visits and detect the early sign and symptoms of COPD to contain the severity of the disease. Telemedicine and telehealth, more specifically home based telecare, have been proven to be very effective in reducing the number of emergency visits and the length of hospital stays in geriatric population and chronically diagnosed patients eventually (Burkow et al., 2015). In addition to managing the acute exacerbation episodes, home based telecare has also been adopted and preferred by the patients for managing the primary and secondary care services (Calvo et al., 2014).
Congestive heart failure and Hypertension
Congestive heart failure of CHF is one of the most prevalent chronic diseases, so much so that one in five American people that have crossed the age of 40 have a complaint of CHF. It is one of the main reasons behind patient’s hospitalization and re-hospitalization, and since these processes are costly, the eventual outcome of CHF is poor despite the modern medications and procedures and like other chronic conditions, the complexity in managing CHF will continue to (Seibert et al., 2008). The usage of telehealth services for managing congestive heart failure allows patients to be more aware of their condition and the risk factors affecting them directly. There has been a significant betterment reported in addressing the home based telecare for CHF patients. Telemedicine helps patient in taking care of them by keeping them in check with their current health status, medication intake and overall weight to keep them healthy. While keeping an eye on their vitals and condition status, patient’s systolic blood pressure has also been shown to improve with the use of telehealth services (Lehmann, 2006).
Arthritis
Telehealth has been proving its worth in places where there has been an increase in physician referrals in relation to the rheumatology cases in areas that are underdeveloped and rural in nature. With the help of videoconferencing technology patients are highly satisfied with the immediate response rate and cost effective method of teleconsultation (Jong & Kraishi, 2004). In addition to this the communication between the referring physician and the rheumatologist is also improved by using the telehealth interface leading to a better and improved outcome in their patients. Although there is a limitation to this mode of healthcare delivery where patients preferring face to face traditional mode of rheumatology consultation, but overall this technology has proved to be resource-saving, faster and easily accessible solution too people living in rural areas with in knee and shoulder pain (Knudsen et al., 2018).
Dementia
Dementia is a neurological disorder that is characterized by forgetfulness, and decreased language, memory and critical thinking ability with aging. It has a slow onset and is irreversible with time. One of the major concerns in people with dementia is the forgetfulness and improper ways to manage their medications. Almost all of the elderly patients diagnosed with chronic dementia opt for nursing care while a very few of them have an in-home care facility. Telecommunication services can be very helpful in monitoring the status of such patients. Telemonitoring by virtual healthcare providers has gained a positive response in both the patients and the nursing community as it increases the social interaction of the patients, lowers caregiver’s concernment, reduces costly forms of care and enhanced medication adherence and improves the life’s quality in general. As dementia is lifelong chronic disease and these services are cost effective hence they can easily be used throughout the life (Smith & Gray, 2009).
Kidney disease
Chronic kidney disease also known as CKD leads to kidney failure, in some patients’ unilateral while in severe cases bilateral, which accounts for the dialysis procedure. Since the kidneys fail to function properly, dialysis which is an expensive treatment that aims at eradicating extra bodily salts, toxins, water and other harmful chemicals that are not required by the body. As it is already an expensive treatment procedure, the expense of travel, taking a leave from work, staying away from family and the increased number of hospital visits can take a toll on the patient’s willing power. Dialysis can be performed at home but the major barrier to this idea is the lack of home care post and during the dialysis hindered by both geographical and socioeconomic factors of the patient (Ishani et al., 2016). On the other hand, telehealth can serve as a very authentic and efficacious tool for home based care post dialysis and also surmount the barriers of geographical barriers and cost issue and improve patient’s clinical outcome. But there is a lack of data available for home based care after dialysis. The main reasons for lack of literature might be the reimbursement issues, lack of education of machineries and technologies used for remote care and the high cost technology used in the dialysis. Remote monitoring of the patients can be done via a Bluetooth device, a telemetry device or through synchronous data share by videoconferencing. Telehome care will not only improve patient’s clinical outcome but also his quality of life, decrease the burden of disease, lower the number of hospitalizations, enhance comfort level and decrease the number of onsite infections since the environment of the home is safe and germs free. However, there is lack of scientific evidence for these benefits and yet at the same time there are few barriers to telehome care as well such as low internet speed, lack of education on remote services and lack of patient and physician acceptance of this technology (Krishna et al., 2017).